deQuervain's
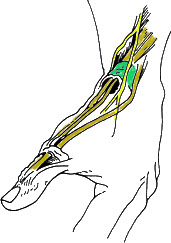
Figure 1
The tendons to the thumb go
under the extensor retinaculum
(green); nerve is in yellow.
DeQuervain’s is a condition brought on by irritation or swelling of the tendons found along the thumb side of the wrist (Figure 1). The irritation causes the compartment (lining) around the tendon to swell, changing the shape of the compartment; this makes it difficult for the tendons to move as they should. The swelling can cause pain and tenderness along the thumb side of the wrist, usually noticed when forming a fist, grasping or gripping things, or turning the wrist. The pain is usually described by patients as a very sharp, stabbing pain. It is not subtle. Although many physicians call this "tendonitis" (which means an inflammatory condition of the tendons), actually inflammation is not a key component of the problem. Read more about the cause of deQuervain's in the next section.
What causes it?
The cause of deQuervain’s is an irritation of the tendons at the base of the thumb, particularly where they go under the extensor retinaculum (see green structure in Figure 1). The irritation is due to a degenerative process in which the body lays down a material called a mucopolysaccharide in the tendon; this process is called "myxoid degeneration." The tendon sheath becomes thicker (up to five times thicker than normal subjects) and does not slide as well as it should. The sheath can also thicken due to increased fibrous tissue and increased vascularity. All of this adds up to a very sharp pain when the patient moves the thumb. Sometimes this is worsened by awkward hand positions or overuse. For example, the position of the wrist during breastfeeding or the frequent lifting of a baby by a new mother in caring for an infant is a common cause of this condition.
While many doctors still describe deQuervain's as an inflammatory condition, it has been shown quite clearly from microscope studies that inflammation is not really a significant part of this problem.
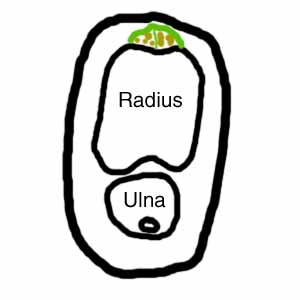
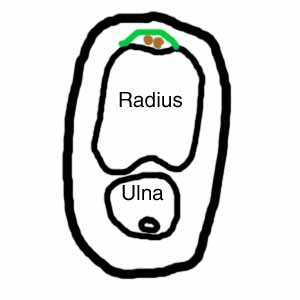
In addition, many patients with deQuervain's have more than the normal number of tendons in this compartment. The figures below are cross-sections of the forearm at the level of the base of the thumb. The figure on the right is the normal situation. The green line represents the ligament that helps to hold the two thumb tendons (shown in brown) down to the radius (the main bone of the forearm). There are usually two tendons. In patients with deQuervains (figure on the left), it is usual to find more than two tendons. Three or four tendons is common, but I have had one patient with five. If there are more than two tendons, it is common for there to be a septum (Latin for "wall") between some of the tendons (shown as a thin vertical green line in the figure on the left). It is thought that the patients who develop deQuervain's have a combination of unusual anatomy plus unusual repetitive use of the thumb, but this is not proven.
 |
 |
Signs and symptoms
Figure 2 Finkelstein maneuver
used to diagnose deQuervain’s tendinitis.
Pain over the thumb side of the wrist is the main symptom. The pain may appear either gradually or suddenly. It is felt in the wrist and can travel up the forearm.
The pain is usually worse with use of the hand and thumb, especially when extending the thumb (the "hitch-hikers" position). Swelling over the thumb side of the wrist is noticed and may be accompanied by a fluid-filled cyst in this region. There may be an occasional catching, grating, or snapping when moving the thumb. Irritation of the nerve lying on top of the tendon sheath may cause numbness on the back of the thumb and index finger, although this is rare.
Diagnosis
The diagnosis of deQuervain's is made in the office by the clinical exam. No special studies (xray, MRI) are needed.
A Finkelstein's Test is generally performed (see Figure 2). In this test, the patient makes a fist with the fingers over the thumb (ie, the thumb is in the palm, under the fingers). The wrist is then bent in the direction of the little finger (Figure 2). This test can be quite painful for the person with deQuervain’s tendinitis. There is also tenderness directly over the tendons on the thumb-side of the wrist. The most important diagnosis to rule out is arthritis of the thumb base, as this can mimic deQuervain's.
Treatment

Figure 3
Surgery opens the sheath over the
inflamed tendons.
The goal is to relieve the pain caused by the irritation and swelling. The condition can be treated by a splint, but it is not very effective, works only because you cannot use your thumb (and who can afford to give up the use of their thumb?), and usually returns as soon as the splint is discontinued. The most effective treatment is a steroid injection. This injection is usually effective in about 82% to 95% of cases.
When symptoms are severe or do not improve, I may recommend surgery. The surgery opens the sheath (seen in green in Figure 3)) to make more room for the irritated tendons. The surgery is done on an out-patient basis. Patients can usually use the hand lightly right after surgery and most patients have normal use within about a month.
During surgery, I also explore to make sure to decompress any extra compartments and extra tendons. The chief surgical complication is irritation of the nerve (see the yellow structure in Figure 3), which is a branch of the radial sensory nerve. Although Figure 3 shows just one nerve, generally there are several (two to four) branches that are located over the sheath, and need to be moved out of the way. This nerve is very sensitive to any handling, so I am very gentle with it. While nerve injury is a possibility, problems with the nerve are actually quite rare (none so far in my career, but I continue to be very careful!). After surgery, it is important to work on wrist range of motion, flexing and extending the wrist, keeping all the fingers and especially the thumb, loose. While doing this exercise, do not simultaneously bend the wrist and also extend the thumb. Thumb exercises should be done with the wrist in neutral (not flexed or extended). his helps to keep the hand flexible but does not risk subluxing the operated tendons from popping out of position. This usually happens when patients fully flex or extend their wrists, then simultaneously doing forceful motions of the thumb.
