Needle Aponeurotomy
First posted July 2, 2003 Last updated December 15, 2015
There are several different surgical techniques that are used to treat Dupuytren's disease, one of them is needle aponeurotomy. This is an old technique which has seen a resurgence in the US in the last few years with a new twist. I have a particular interest in Dupuytren's, since I have it myself, so I have been paying very close attention to developments in this field.
The founder of hand surgery in the US was Sterling Bunnell, MD, who lived in Tiburon and practiced in San Francisco. He and his partners did a type of aponeurotomy, using a scalpel. I have actually watched the last surviving partner of Sterling Bunnell, Dr. Robert Brown, do an aponeurotomy in his office just down the street. I don't believe anyone is still doing that particular technique, due to its risk of complications.
The modern variation, needle aponeurotomy, was developed by Dr. Jean-Luc Lermusiaux, who is a rheumatologist practicing at the Hopital Laribosiere, in Paris, France, in the 1950's. It was introduced into the US by a friend of mine, Dr. Charles Eaton, in Florida. I have spoken to Dr. Eaton about needle aponeurotomy many times and I am fairly knowledgeable about it.
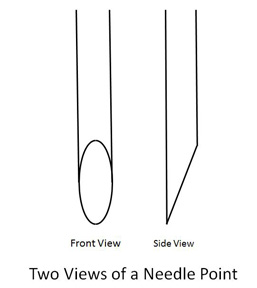
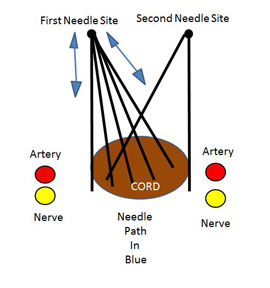
Dr. Eaton went to France, learned the technique, brought it back to the US, and since has been training US surgeons. The technique involves using a standard hypodermic needle to cut the cords of Duputyren's. See the image above. On the side view, you can see that the needle is shaped like a very small, very thin scalpel, which can be used to cut the cord by swiping it back and forth (see image below).

In my illustration, the Dupuytren's cord is in brown, the finge arteries are red and the finger nerves are yellow. The needle, being used as a small scalpel, is inserted at the first needle site vertically, and then swiped as shown by the blue arrow (for the first needle site only). The neede is then inserted at the second needle site and the swiping repeated. The intention is to cut the cord.
The advantage of the technique is that it is done in the office, the return to activities is rapid, and hand therapy is not needed. The disadvantage of the technique is that it is done blindly, that is, the skin is not opened and the nerves and arteries that lie alongside the Dupuytren's cords are not seen, the Duputyren's tissues are not removed, and the recurrence of the contractures is more rapid.
Contractures return in essentially all patients, despite what some websites claim. This is in part because the underlying problem of Dupuytren's lies in the fact that it is a genetic disease and every cell in the body has the genes for it. Over time, more and more cells manifest the disease. That is, cells which were not involved in the disease at one time become involved in the disease at a later time.
Even open surgery results in the contractures coming back. Needle aponeurotomy results in the contractures coming back more quickly, due to the fact that the original contracted tissues are not removed. How much more quickly? This is a very important question, but at this time, there is limited evidence to telll us how longs. Based on best evidence, it is probably 2 or 3 years, according to Dr. Eaton and others. According to a study presented at a national surgery meeting by one of the surgeons involved in a study of needle aponeurotomy, the change of a finger getting a contracture of recurrence of >20 degrees was 14% at the knuckle (the third joint down from the fingertip, called the metacarpal-phalangeal joint, or MCP) and 54% in the second joint down from the fingertip (called the proximal interphalangeal joint, or PIP), at 2.5 years. The surgeon did not study the patients for longer than 2.5 years, but estimated that the recurrence rate of a contracture >20 degrees would be between 60 and 70%. I contrast, I would estimate that open fasciectomy may never need to be repeated in about 30% of patients, and some (50%?) may need it again in 5 to 10 years, but most patients will be at the higher end of this range.
It is important to understand the difference between recurrence and extension. While they both mean that the contracture came back, there is an important difference in how they came back. Recurrence refers to the situation in which the contracted tissues remain in the hand, which occurs in both needel aponeurotomy and in collagenase injections. Extension refers to the situation in which previously uninvolved tissues now express the Dupuytren's gene and are now showing the disease. The contractures come back in needle aponeurotomy because of both recurrence and extension. The contractures come back after open fasciectomy because of extension only. This cannot be prevented until we have a genetic treatment for Duputyren's disease.
Due to the disadvantages of the rare injuries that can occur with needle aponeurotomy, the lack of removal of the Duputyren's tissue, and the more rapid return of the contractures, most US surgeons are not performing needle aponeurotomy very frequently. Most who perform it have only been doing it a short time and do it on only selected cases. Dr. Eaton presented a symposium on the technique at the American Society for Surgery of the Hand in about 2006, but did not present followup on the patients. The hand surgery community would like to know the complication rate (cut nerves and arteries) and the recurrence rate (known to be quicker than the standard, open fasciectomy). Despite denials of complications by several surgeons who do needle aponeurotomy, other surgeons have reported repairing both cut nerves and cut arteries by practitioners of needle aponeurotomy, even some of the ones who are advertising on the Internet. This has happened in Europe, in the US, and even here locally in Marin. I remain quite skeptical of claims of no complications with needle aponeurotomy, based on my own observations and those of other hand surgeons. If a nerve is cut, it is repaired but it will never be normal; some numbness and possibly pain will exist for the life of the patient.
Dr. Eaton has developed a new technique of needle aponeurotomy that decreases the risk of damage to nerves and arteries, and has taught it to me. It involves moving the needle mostly up and down like a sewing maching and very little in the way of the classic side to side swiping. I have been very please with the results in my own patients. (See image below.)
It is important that you recognize that not all cases of Dupuytren's disease is treatable by needle aponeurotomy. It is most appropriate for simple cords that are well-defined in the palm with soft, mobile overlying skin. It is least appropriate for extensive disease, contracted skin, contracted finger joints, and cords that are over the metacarpal-phalangeal joint (the "knuckle" of the hand).
I myself have Dupuytren's, but it does not yet need surgery. I have done needle aponeurotomy on a few patients who have a simple palmar cord that is elevated (away from the nerve and the artery) and a contracture of the MP joint (the "knuckle"). Knowing what I know about the risks, benefits, and outcomes of both needle aponeurotomy and open fasciectomy, and knowing what kind of great results I get in my own patients with the open technique, if a patient has more than a simple palmar cord, I would recommend open fasciectomy and that is what I would want for my own hands.
If you want to read about needle aponeurotomy by my friend, Dr. Charles Eaton, click on this link: Dupuytren's Disease.
