Lunotriquetral Instability

David M. Lichtman, MD
Reported by David Nelson, MD May 20, 2000; illustrations modified from multiple sources by David Nelson, MD
Reviewed by David Lichtman, MD
David M. Lichtman, MD
JPS Health Network, Chairman/Director, Dept of Orthopaedic Surgery, Orthopaedic Residency Program, Fort
Worth,Texas
Clinical Professor of Orthopaedic Surgery, U.T. Southwestern Medical Center, 5323 Harry Hines Blvd., Dallas, Texas
Adjunct Professor, Department of Orthopaedic Surgery, Baylor College of Medicine, Houston, Texas
Professor, Department of Surgery, Uniformed Services University of the Health Sciences (USUHS), Bethesda, MD
First Description
The first description of lunotriquetral instability was by Reagan, Linscheid, and Dobyns in their 1984 paper, Lunotriquetral Sprains. They classified triquetral injuries into sprains and dissociations. Sprains were defind as injuries that did not cause a displacement of the bones. Dissociations were a rupture of the lunotriquetral ligament.
 |
 |
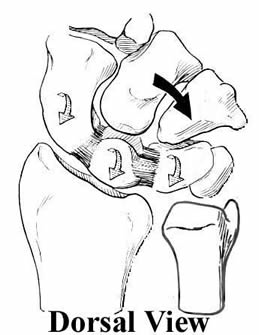
They built on the concepts established in the American literature by Dobyns and Linscheid, in their classic paper, Traumatic Instability of the Wrist. This paper noted that the proximal row was an intercalated segment, and that its position depended on the influence of the scaphoid causing proximal row flexion with radial deviation, and the triquetrum causing proximal row extension with ulnar deviation (shown here, modified by Nelson, from an illustration in The Wrist: Diagnosis and Operative Treatment, by Cooney, Linscheid and Dobyns).
Lunotriquetral Dissociation
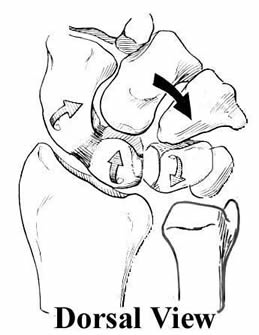
Reagan, Linscheid, and Dobyns stated that LT dissociation was a separation of the bones that resulted in a lack of coordinated proximal motion: the triquetrum moves independantly. In radial wrist deviation, the scaphoid would pull the proximal row into flexion with the triquetrum staying extended. In ulnar deviation, as shown here, the triquetrum wold move into extension, but that this extension moment would not be communicated to the scaphoid and lunate, which would stay in flexion, creating the so-called VISI deformity. (Illustration modified by Nelson, from The Wrist: Diagnosis and Operative Treatment, by Cooney, Linscheid and Dobyns). (In an interesting footnote to history, Linscheid, Dobyns, et al. in 1972 called this PISI, for palmar intercalated segmental instability; this was changed without fanfare in following publications to VISI, a more polite-sounding name - Nelson)
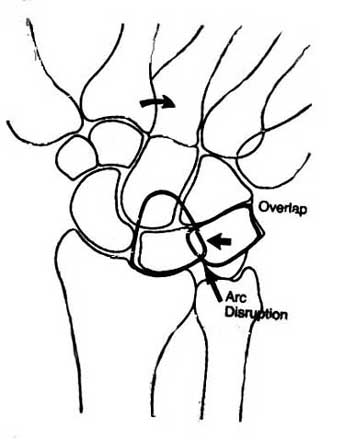
The dissocation between the lunate and triquetrum can also be seen in the change of the lunate profile (from four-sided to three-sided) and sometimes in a break in Gilula Arc I (shown here, modified by Nelson, from The Wrist and Its Disorders, by Lichtman and Alexander). (Note: this is not a reliable sign, according to Gilula, who has noted that 95% of wrists have a break at either Arc I or II with radial or ulnar deviation: see Normal Disruption of Carpal Arcs - Nelson).
Three Part Classification
This classification can be further divided, by classifying LT injuries into three parts:
1 sprains (pre-dynamic instability)
2 partial dissociation (dynamic instability)
3 dissociation (static instability)
Lichtman credited H. Kirk Watson with coining the terms "pre-dynamic instability", "dynamic instability", and "static instability". These are based on the appearance of the lunate and triquetrum on xray. In sprains, no dissociation can be seen with stress views. In partial LT dissociation, stress views demonstrate a gap between the bone. In LT dissociation, the gap is apparent on plain xrays.
Anatomic Basis for Three Part Classification
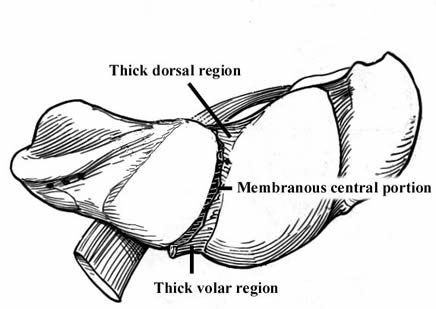
Sprains are due to tears in the central, membranous portion of the ligament. Partial dissociation is due to a tear in the central as well as either dorsal (more common) or volar ligment. Complete dissociation is due to a tear in all three regions, as shown at right (modified by Nelson, from The Wrist: Diagnosis and Operative Treatment, by Cooney, Linscheid and Dobyns).
Three Etiologies of LT Dissociation
There are three normal causes for LT dissociation:
1 Mayfield-Johnson stage III perilunate dislocation, with supination and radial deviation
2 isolated traumatic event with intercarpal pronation and ulnar deviation (this is the reverse of a Mayfield-Johnson injury)
3 ulnocarpal abutment syndrome (Palmer)
Diagnosis
The diagnosis almost always can be made on the physical examination and plain radiographs. The Linscheid ballottement test for the LT joint should reproduce the patient's pain. Careful examination should also allow you to differentiate clunks, click, snaps, and grinds. Clunks are low frequency sounds, due to subluxation and relocation. Clicks are higher pitched sounds, due to two bones rubbing against each other. Snaps are very high pitched sounds, due to tendons slipping around obstacles. Grinding or crepitus is usually due to synovitis.
Arthrograms were initially the definitive tests, but have been shown by multiple authors (see The relevance of ligament tears or perforations in the diagnosis of wrist pain: an arthrographic study by Peter Stern - Nelson) to have a very high rate of false positives and a non-negligible rate of false negatives. MRI has been suggested as a way to examine wrist ligaments, but they rarely are of sufficient quality to allow a definitive judgement to be made. (See also: The importance of the physical examination for further information about both the physical exam as well as MRI - Nelson)
The current definitive diagnostic test is wrist arthroscopy, which allows diagnosis, staging, and for some cases, even treatment.
Treatment
LT Sprain
LT sprains can often be treated by debridement during wrist arthroscopy, sometimes with the addition of ulnar shortening in cases of ulnar plus wrist (usually > 2 mm +). Shortening can take many forms, including a Feldon wafer procedure or formal ulnar shortening. A oblique osteotomy usually works best and tends to avoid the most common complication of nonunion. The importance of evaluating the wrist for ulnar variance and treating the ulnar plus wrist cannot be overemphasized.
LT Partial Dissociation
Direct repair, when possible, is the best choice. It is usually avulsed off the triquetrum and is still attached to the lunate.
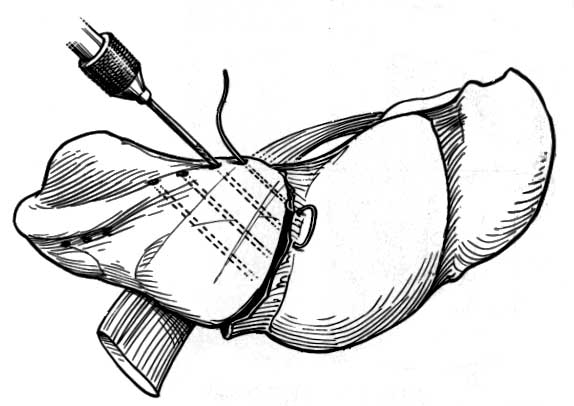
(The artist has a much better success rate at the procedure than the surgeon, and don't expect your repair to look like that at the right, from The Wrist: Diagnosis and Operative Treatment, by Cooney, Linscheid and Dobyns. - Nelson)
LT Dissociation
These injuries can usually be treated as for partial dissociations if they are caught soon enough, but that is usually the biggest problem. These injuries are usually not recognized by the general orthopedists, and the referral often comes too late for an acute repair.
Chronic LT Dissociation
The chronically dissociated LT joint is much harder to treat. Soft tissue procedures have not worked well for me, and fusion is the best choice. The manner of fusion has been reviewed in the literature, with various types of morsellized cancellous vs. cancellous strut grafting, and various types of internal fixation being used (K-wire vs. Herbert or Acutrac screws). The literature demonstrates that fusion is possible if attention is paid to fully decorticating the dorsal 2/3 of the joint space (leave some intact to prevent graft migration), internally fix, and then immobilize the patient (two to three months). Nelson and Manske, and Pin and Weeks demonstrated that screw fixation was superior to K-wire immobilization.
Berger and Bishop have published a technique of capsular reconstruction, but they have not convinced me that their results are better than LT fusion. I reviewed their paper at the ASSH in Boston. There were multiple surgeons over a period of 20 years doing the fusions, and then they compared this group to their more recent experience with capsular reconstruction. This was not a fair comparison. A prospective study would be required to establish their hypothesis.
Summary
In summary, debride the sprains, repair the partial dissociations, and fuse the chronic complete dissociations, and never forget to treat the positive ulnar variance, no matter what the LT injury proper is.
Reported by David Nelson, MD May 20, 2000
Reviewed by David Lichtman, MD
This talk was sponsored by unrestricted educational grants from Norcal Mutual Insurance Company, a medical malpractice insurance company; and by Merck, makers of Vioxx. Neither company has any financial interest in any aspect of the topic of this presentation.
