Complex Regional Pain Syndrome
Reflex sympathetic dystrophy (RSD), currently better named Complex Regional Pain Syndrome
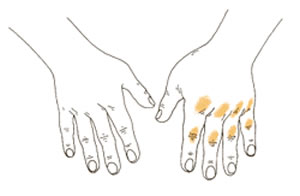
Figure 1
On the right, the swollen, painful hand of early CRPS
with reddened joints.
(CRPS), is a syndrome (collection of symptoms) that is characterized by burning pain (can vary from mild to severe), stiffness in the affected joints of the extremity, swelling, discoloration, skin changes (thinness, shinyness, excessive sweating, hair changes), bone changes (osteoporosis), and extreme sensitivity to light touch. The severity of the symptoms can also vary widely, from just a little vasomotor changes (variation in the color of the skin from moment to moment, due to constriction of blood vessels) to rather disabling pain and almost complete joint stiffness, resulting in a useless hand or foot (the usual affected parts of the body). The rest of this discussion will only deal with CRPS of the hand and upper extremity, since this is the only part of the body I treat and have experience with. The disorder is unique in that it simultaneously affects the nerves, skin, muscles, blood vessels, and bones. One good aspect of CRPS is that the problem is self-limited (will eventually resolve by itself), although treatment can help hasten the resolution and decrease the permanent effects of it (primarily stiffness).
CRPS has been called many things in the past (RSD, casualgia, Sudeck’s atrophy, and shoulder-hand syndrome). Causalgia was first documented in the 19th century by physicians concerned about pain Civil War veterans continued to experience after their wounds from high-velocity impacts such as those from bullets or shrapnel.had healed. Doctors often called it "hot pain," after its primary symptom. Complex Regional Pain Syndrome, or CRPS, is a better term because research has shown that it is more complex than just a reflex in the sympathetic nervous system. It is due to a perception of pain and other noxious input to the brain that is sustained long after the initial insult to the body has ceased. Research and clinical evidence indicates that the original injury probably occurs due to an injury to the sympathetic nervous system. (The sympathetic nervous system controls the automatic processes of the body, such as heart rate, blood flow, the stomach and intestines, and sweat glands, among other things.) When the nervous system becomes overactive, burning pain is felt and swelling and warmth are left in the affected arm. If not treated, CRPS can cause stiffness and loss of use of the affected part of the arm.
The International Association for the Study of Pain (Dr. Nelson is a member and has contributed original research to their meetings) recognizes two sub-types of CRPS: Type I (which corresponds to classic RSD) and Type II (which corresponds to causalgia).
What causes CRPS?
This is a much more complex question than you may realize, and it is an area of vigorous research that is targeted and supported by the National Institutes of Health. In some cases, the cause of CRPS is unknown. Why any one particular injury will result in CRPS and another similar injury to the same patient did not, is not clear. Why one particular surgery will result in CRPS, when hundreds of seemingly identical surgeries in other patients did not, is unknown. To say that CRPS developed "after" a surgery also does not answer the question of "what caused the CRPS?" "After" does not mean "because of" (for those of you interested in Logic, this is the "post hoc, ergo propter hoc" fallacy), nor does it tell us anything of the mechanism of its causation.
Often an injury such as a fracture or a laceration can cause CRPS, or the symptoms may appear after a surgery. The onset of symptoms is not immediate, and may lag about 3 weeks or so from the event that we think probably caused it, so identifying the cause can be difficult to impossible. Other causes include pressure on a nerve, infection, cancer, neck disorders, stroke, or heart attack. We think that the common event in all of these conditions is a painful injury, probably involving a nerve. It is theorized that these damaged nerves send inappropriate signals to the brain, interfering with normal information about sensations, temperature, and blood flow. The incidence of CRPS does not seem to be more common after large injuries, and can follow even relatively minor injuries that do not obviously involve a nerve.
Until recently, doctors thought that CRPS always involved a problem in the sympathetic nervous system (as I noted above, the sympathetic nervous system controls the automatic processes of the body, such as heart rate, blood flow, the stomach and intestines, and sweat glands, among other things.) They also thought that the problem involved a reflex arc, from the injured part to the spine and back to the arm. This is where the term "Reflex Sympathetic Dystrophy" came from. (The "dystrophy" part came from the muscle atrophy that developed in untreated arms.) Research has shown that, while this may explain some cases, it does not explain all, or possibly even most, cases.
If SMP does not explain the pain in most patients with CRPS, what is the cause of the pain? Experts agree that there are problems in the peripheral nervous system (the nerves in the body) and the central nervous system (the brain and spinal cord) of patients with CRPS, but the details are not known. There are other factors that could be involved in the development of CRPS because they directly affect the activity of the nervous system, muscles and bones. Examples of these factors are emotional issues or stress (see section below on personality types) and not using a painful body part. One thing we know for certain: many pathological processes are at work, the condition affects more than one organ system in the extremity, and that pain is the predominant symptom experienced by the patient. This is why the term "Complex Regional Pain Syndrome" is a better name than "Reflex Sympathetic Dystrophy". RSD, however, is such a well-established and widely-used term, it will not disappear from the medical vocabulary.
We now know much more about the sympathetic reflex, and this sort of pain is now called "sympathetically maintained pain", or SMP, and is found in other conditions as well. The only way a doctor can find out if a patient has SMP is to do a sympathetic nerve block. (Sympathetic nerve blocks are injections of a numbing drug, called a local anesthetic, into different sites in the body). A person suffering from CRPS can be said to have SMP only if he or she has good pain relief from a sympathetic block.
Signs and symptoms
Figure 2
This diagram shows how a nerve
injury may cause a “short circuit”
in the nervous system resulting in
sympathetic over activity in the hand
with burning pain, swelling, and increased
sweating.
The symptoms of CRPS usually occur near the site of an injury and include: burning pain, muscle spasms, local swelling, increased sweating, joint tenderness or stiffness, restricted or painful movement, and changes in the nails and skin. One visible sign of CRPS near the site of injury is warm, shiny red skin that later becomes cool and bluish. The pain that patients report is out of proportion to the severity of the injury and gets worse, rather than better, over time. It is frequently characterized as a burning, aching, searing pain, which may initially be localized to the site of injury or the area covered by an injured nerve but spreads over time, sometimes involving an entire limb. Pain is continuous and may be heightened by emotional stress. Moving or touching the limb is often intolerable. If untreated, the joints may become stiff. As you can imagine, there can be significant psychological effects of CRPS, due to the severe and chronic nature of the pain and disability.
The symptoms of CRPS vary in severity and duration, with the majority of cases being very mild, with more stiffness and tenderness than would be expected after an injury such as a distal radius fracture. However, some rare cases can be severe. There are usually three stages associated with CRPS, and each stage is marked by progressive changes in the skin, nails, muscles, joints, ligaments, and bones.
The pain associated with reflex sympathetic dystrophy is often described as burning in nature. Swelling can cause painful joints and stiffness. The color of the skin can vary from reddish to purplish to pale, varies with the stage of the disease, and can vary by the minute.
RSD has three stages
Stage I (acute) usually starts after a delay of three or four weeks and lasts up to about three months. During this stage the symptoms include pain (usually described as a burning pain, which can be severe) and swelling, increased warmth in the affected part/limb, and excessive sweating. There may be faster-than- normal nail and hair growth and joint pain during movement of the affected area (Figure 2). An unusual aspect of CRPS is how it can affect the muscles that control the diameter of skin blood vessels. The innervation of the muscles is probably the reason for the condition, and the nerve impulses to the blood vessels can rapidly vary, with the result that the skin color can vary from pale to red or bluish in a matter of a minute or so. This is called vasomotor instability.
Stage II (dystrophic) can last three to six or twelve months. The pain is often increased and can be more widespread. The hand or arm can be more sensitive to touch. Swelling is more constant, skin wrinkles disappear, skin temperature becomes cooler, and fingernails become brittle
Stage III (atrophic) occurs from one year on. The skin of the affected area is now pale, dry, tightly stretched, and shiny. The area is stiff, pain may decrease, and there is less hope of getting motion back.
It should be noted that recent research has challenged the concept of CRPS progressing through stages (see the official journal of the International Association for the Study of Pain, Pain, Vol 95, No.s 1-2, January 2002, page 119-124, Complex regional pain syndrome: are there distinct subtypes and sequential stages of the syndrome?" These authors found in a study of 113 patients that symptoms were stable and did not progress through 3 stages, but that the IASP's two sub-types did exist. More research is ongoing. For now, there is some utility in the concept of stages, but you should be aware that it may not be the best description of the disease.
Who gets CRPS?
Anyone who has an injury or surgery (either elective or for an injury) can develop CRPS. However, there do seem to be certain things which may increase the incidence of CRPS. It is more common with injuries to nerves or injuries that are very painful (probably involving an unrecognized nerve injury) , often between the ages of 40 and 60. It affects both men and women, but is most frequently seen in women. It affects all personality types, but seems to be more common in Type B (passive) personalities than in Type A (active) personalities, although this categorization of people's psychological makeup is rather crude and may not be of much value. My professional experience supports this general concept; however, I have had two very strong Type A patients who have gotten severe CRPS. Investigators estimate that two to five percent of those with peripheral nerve injury may develop CRPS.
Diagnosis
The diagnosis usually is made when at least three of the following symptoms are present: pain and tenderness, signs of changed blood flow (either increased or decreased), swelling with joint stiffness, or skin changes. The prognosis is good if the CRPS is diagnosed early and treated aggressively. The confusing nature of the condition and it causes as well as its variable presentation often leads to a delayed diagnosis. It is not easy to either diagnose or treat. Many physicians do not have the patience to deal with the complexity of the condition, the patient, and the treatment.
Treatment
Early diagnosis and treatment are important. Three forms of treatment may be combined: medication, physical therapy, and surgery. Medication taken by mouth can help decrease the symptoms. To reduce symptoms and provide long term relief, local anesthetics may be injected into a nerve bundle at the base of the neck (stellate ganglion block). In some cases, a tourniquet is applied to the arm and medication can be injected into a vein along with an anesthetic. Your hand surgeon may recommend therapy by a hand, occupational or physical therapist, or physician. Therapy is important to regain function and reduce discomfort caused by RSD.
Successful treatment depends upon the patient’s full and active effort in therapy. Occasionally surgery is performed in the later stages, but the results can be disappointing. This is certainly a case where good patient education and teamwork between the doctor, the patient, and the certified hand therapist is important in obtaining good results.
There are RSD support groups
You can find them at the end of the page by the National Institute of Neurological Disorders and Stroke, listed below.
~ Modified from documents by American Society for Surgery of the Hand, NIH RSD webpage, International Association for the Study of Pain, and other sources; only Dr. Nelson is responsible for this content.
For a patient's own narrative about living with and overcoming RSD, click here.
National Institute of Neurological Disorders and Stroke has a very professional and well-written site (although I find the historical note on RSD and gunshot wounds from the Civil War rather quaint!)
There is a RSD society. I have reviewed the contents on May 31, 2002, and it seems like reliable content. You may want to discuss what you have read with me, to be sure you understand it correctly and that I feel that it is still accurate. Note the warning below.
